| Improvement of Renal Perfusion and Function by Pneumatic External Counterpulsation. D. Werner et al European Heart Journal 1998;19(Abstract Supplement) P3660(655). How does EECP effect the kidneys? Will EECP improve or compromise blood flow to the kidneys? What happens to kidney function? These are important questions, as many of our patients with recurrent coronary disease also have impaired kidney function. |
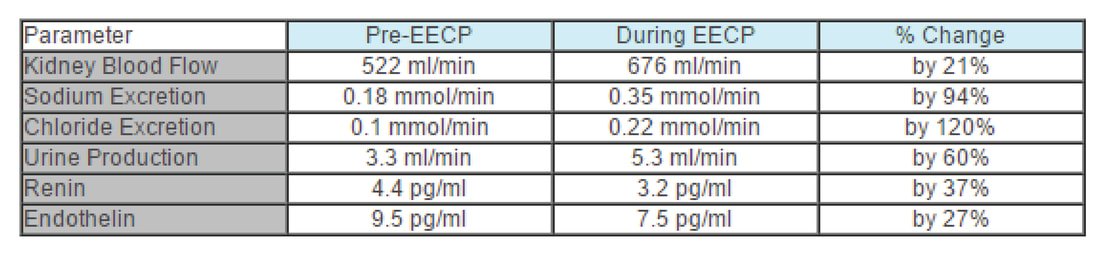
Using a non-invasive ultrasound technique, Werner measured blood flow to the kidneys before and during EECP in 9 healthy volunteers. Parameters of kidney function were assessed in 12 others. Their findings are summarized in the table and discussed below:
B. One of the jobs of the kidney is to remove salt from the body, so excretion of the components of salt, sodium and chloride, serve as a measure of kidney function. During EECP, sodium excretion nearly doubled, from 0.18 to 0.35 mmol/min; chloride removal increased likewise from 0.1 to 0.22 mmol/min.
C. Urine is composed of body wastes, byproducts of metabolism that have toxic effects if allowed to remain in the body. The kidney filters these waste and excretes them in the urine, so urine production rate serves as a good measure of overall kidney function. Werner found that urine production increased by 60% during EECP, from 3.3 to 5.3 ml/min. This is why you feel the need to empty your bladder during EECP - because your kidneys are working better.
D. Renin is a kidney produced hormone that plays a key role in salt and fluid balance and blood pressure control. When renin levels are high, sodium and water are retained, and blood pressure rises. When renin levels are low, sodium and water are excreted, and blood pressure falls. When blood flow to the kidneys is impaired, the kidneys will produce more renin. Salt retention will occur, expanding the blood volume. Blood pressure will rise, increasing blood flow to the kidneys. Blood flow to the kidneys and kidney function will improve, but the rest of the body pays a price. The elevation in blood pressure strains the heart and increases the patient's risk of stroke. The salt and water retention may lead to edema formation or an aggravation of congestive heart failure. When it comes to renin production, the kidney "cares only about itself". This is why patients with poor kidney function or impaired blood flow to the kidneys as a result of cardiovascular disease typically have elevated renin levels, high blood pressure, and a tendency towards fluid retention, edema, and congestive heart failure. On the other hand, when the kidneys are receiving an adequate blood flow, they begin to produce less renin, and good things follow. Blood pressure falls, decreasing stroke risk and the heart's workload. With less fluid retention comes an improvement in edema and a decreased tendency towards CHF. For the cardiac patient, an elevated renin level is bad, and any intervention that lowers renin is to their benefit. During EECP, renin levels fell by 37%, from 4.4 to 3.2 pg/ml.
E. Endothelin is nasty stuff. It constricts arteries. It constricts the coronary arteries, compromising blood flow to the heart. It constricts peripheral arteries, raising blood pressure, increasing the heart's workload. We want a low endothelin level, especially if we have coronary artery disease. Werner found that endothelin levels fell by 27% during EECP, from 9.5 to 7.5 pg/ml.
To summarize, in healthy volunteers (and presumably in patients), EECP:
1. Increases blood flow to the kidney
2. Improves the ability of the kidney to produce urine
3. Promotes excretion of sodium and chloride
4. Lowers levels of the harmful hormones renin and endothelin