|
Improvement of Renal Perfusion and Function by Pneumatic External Counterpulsation. D. Werner et al European Heart Journal 1998;19(Abstract Supplement) P3660(655).
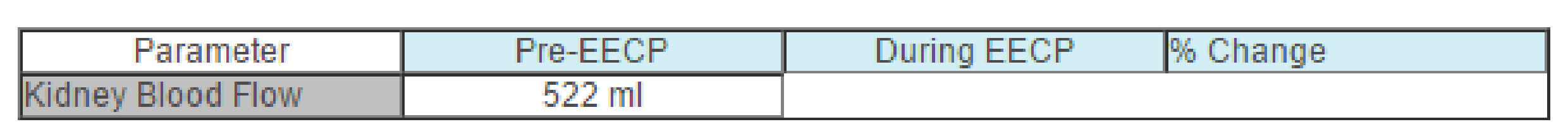
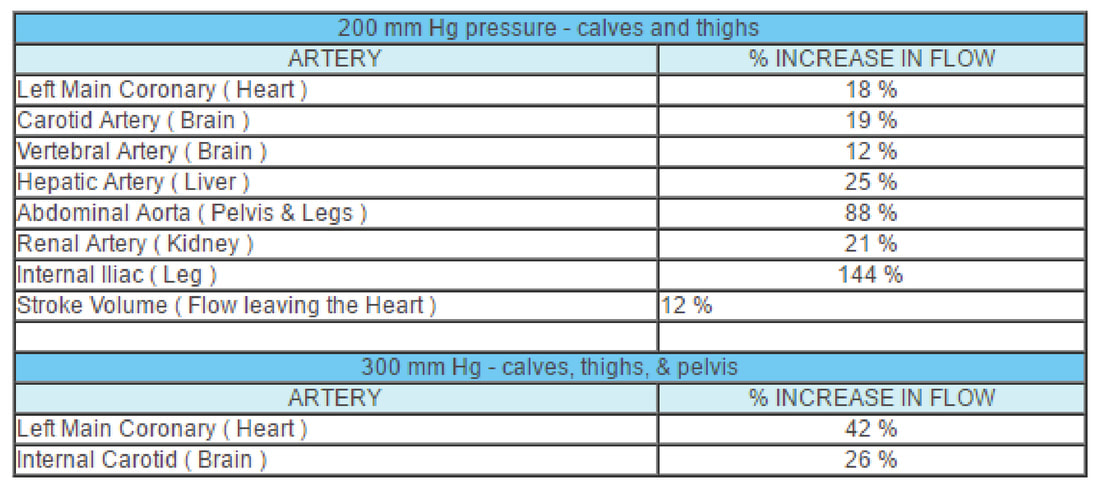
How does EECP effect the kidneys? Will EECP improve or compromise blood flow to the kidneys? What happens to kidney function? These are important questions, as many of our patients with recurrent coronary disease also have impaired kidney function. In these patients, the X-ray dye that we use during angiography and angioplasty can sludge up in the kidneys, compromising kidney function further; full blown kidney failure can rarely occur. In this group, we might turn to EECP as a safer means of reducing angina, but we need to be sure that EECP also won't harm the kidneys. Intuitively, one would predict that EECP would have a beneficial effect on kidney function. The American studies discussed above show that EECP increases blood flow to the heart and improves heart function. Blood flows through native arteries, vein grafts, and arterial grafts increases, and heart function, as measured by treadmill time, nuclear scanning, and angina frequency, also improves. Chinese studies tell us that blood flow to the brain increases with EECP, leading to an improvement in brain function in certain patients. Werner and colleagues set out to study the effect EECP has on blood flow to the kidneys and how this might affect kidney function. Using a non-invasive ultrasound technique, Werner measured blood flow to the kidneys before and during EECP in 9 healthy volunteers. Parameters of kidney function were assessed in 12 others. Their findings are summarized in the table and discussed below: Pneumatic External Counterpulsation: A New Noninvasive Method to Improve Organ Perfusion. Werner, D, The American Journal of Cardiology 1999;84:950-52 In China, EECP is not confined to the treatment of coronary insufficiency. Stroke, cerebrovascular insufficiency, hepatitis, and even diabetes have been addressed with external counterpulsation with measurable benefits. Why should this be? We know that all of these disease states involve free radical tissue damage. Dr.Quan, in article 7, is going to show us that EECP has a significant antioxidant effect. EECP increases blood flow to the coronary arteries that serve the heart. Could an increase in blood flow, with an attendant increase in oxygen and fuel supply to the diseased organ be a mechanism of benefit? Werner and colleagues set out to measure the effect of EECP on blood flow to different organ systems. They used doppler ultrasound (as in Dr. Katz's study - article 1) to measure blood flow per heart beat at rest, during EECP using calf and thigh cuff inflation, and during EECP using calf, thigh, and lower abdominal/pelvic cuff inflation (the method we use in the US). Here's what they found: EECP increases blood flow everywhere, not just to the heart. Organ dysfunction present on the basis of reduced blood flow could thus improve during EECP. In China, arm cuffs are utilized, further increasing blood flow to the brain, and in this fashion EECP is used in the treatment of stroke.
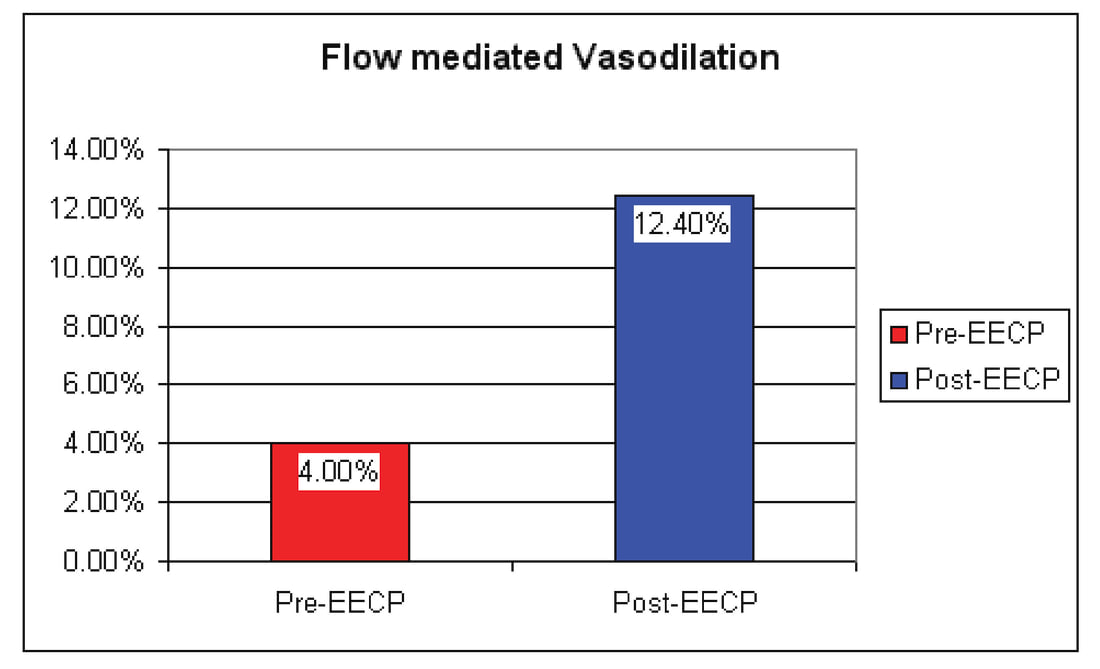
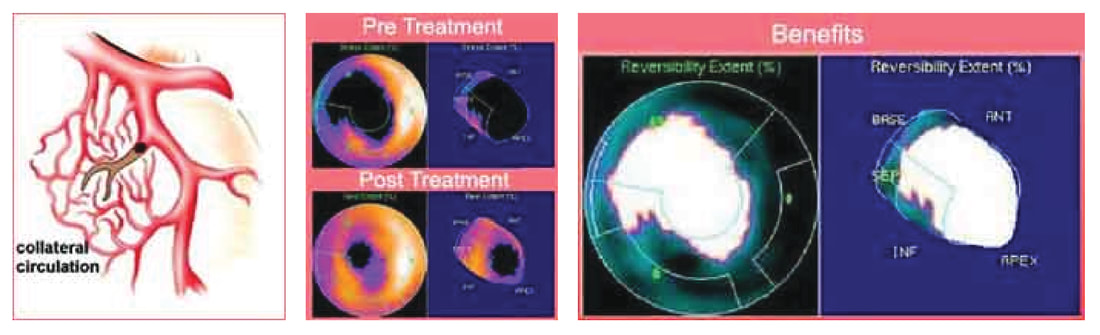
This ability of EECP to improve blood flow in general may lead to some additional applications of EECP in this country - research is ongoing and much more is planned Is it true that EECP restores the function of heart blood vessels - How do we know this for sure?11/5/2018 Intermittent Shear Stimuli by Enhanced External Counterpulsation (EECP) Restores Endothelial Function in Patients with Coronary Artery Diseases. Urano, H, Circulation 102:18 Suppl. II Oct. '00 "As goes the endothelium, so goes the patient" is a scientifically correct statement. The endothelium refers to the thin layer of cells that line our arteries and veins. These cells are essentially tiny hormone and angiochemical producing factories. They make the "good guys", nitric oxide and VEGF, which promote vascular wall integrity, blood vessel vasodilation, and the growth of new vessels. The endothelium also makes "bad guys", such as endothelin, which promotes vasoconstriction, abnormal clotting, and plaque deposition. Endothelial health determines whether the good guys or bad guy angiochemicals will dominate, and has been shown to be a key indicator of cardiovascular health and long-term outcome. We can accurately assess endothelial health by measuring brachial artery flow mediated vasodilation. Here we measure the diameter of the brachial artery (the major artery to the arm at the level of the elbow), before and after release of a blood pressure cuff, which had been inflated enough to impair flow to the forearm for five minutes. As blood flow is restored to the forearm, the brachial artery will dilate by 10-12% to accommodate this increased flow, if endothelial function is normal. If endothelial function is mildly impaired, flow mediated vasodilation will be less than 10%. In patients with established cardiovascular disease, or risk factors for cardiovascular disease such as hypertension, smoking, or high levels of homocysteine or LDL cholesterol, endothelial function may be severely impaired, and the brachial artery will actually constrict. Indeed, endothelial dysfunction may be a final common pathway through which many of the causes or cardiovascular disease actually cause cardiovascular disease. Multiple studies have shown that the health of the endothelium at a given point in time is a critical determinant of the cardiovascular health and vital status of the patient 2 to 5 years later. Whether we are looking at patients with angiographically normal coronary arteries and spasm, individuals with non-obstructive atherosclerosis, or patients with obstructive multi-vessel disease, those with preserved endothelial function do well, while those with impaired endothelial function at baseline are at increased risk for a future adverse cardiac event. The worse the endothelial function, the greater the likelihood that an event will occur. So far, treatments that improve endothelial function have been shown to improve outcome. Accupril, a prescription agent, improves endothelial function by blocking endothelial bound ACE, a nitric oxide degrader. Accupril decreases restenosis after angioplasty or stent placement, and the QUO VATUS study showed us that Accupril decreases one-year post-CABG event rate by 80%. Vitamin E blocks endothelial superoxide, another nitric oxide degrader; the CHAOS study demonstrated that vitamin E, begun after angiography, reduced two year event infarction/death rate by 47%. During exercise blood flow velocity and quantity increase, exerting a radial shearing stress on the endothelium. A healthy endothelium, and to a somewhat lesser extent an unhealthy endothelium, will respond by elaborating more nitric oxide. Nitric oxide will in turn improve endothelial function, dilating the vessel to accommodate the increased flow, and will promote collateral generation. Exercise leads to an increase in nitric oxide and multiple studies have shown that regular exercise improves outcome - this is why cardiac rehab programs are so helpful. To answer this question, Urano measured flow mediated brachial artery vasodilation, a reproducible, accurate measure of systemic and coronary endothelial function, before and after a 35-hour course of EECP, given to stable angina patients with documented coronary disease and abnormal stress EKG studies. The patients' clinical status and treadmill findings improved, consistent with all prior studies. Flow mediated brachial artery vasodilation, significantly impaired at baseline at 4%, improved 3-fold following EECP to 12%, essentially a normal value. It's becoming clear that EECP decreases symptoms and improves outcome not just by forcing open collaterals, but also by improving the patient's biochemistry and endothelial function.
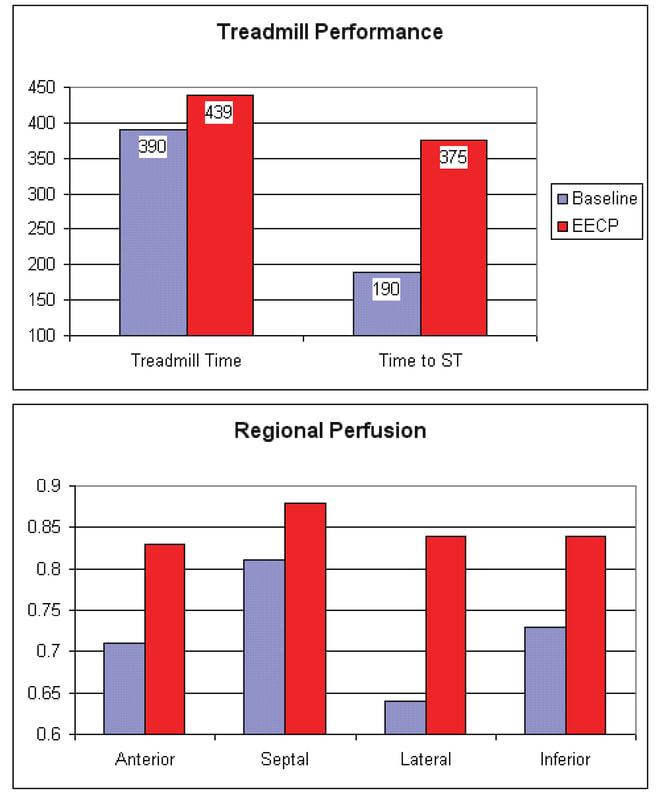
It hasn't been studied yet, but it is my impression that measures designed to improve endothelial function, such as tissue specific ACE inhibitors, arginine, omega-3 essential fatty acids, and anti-oxidants, improve and extend the patient's response to external counterpulsation. These agents all have beneficial effects on their own, so now I typically place new EECP patients on an "endothelial cocktail" of these treatments, and continue it post-EECP. 10a. Endothelial function in patients with severe coronary artery disease treated with enhanced external counterpulsation (ECPT). Schechter, M, et al. European Heart Journal (2002) 23 (Abstract Supplement) - P2363, page 463. Urano's study, abstracted above, demonstrates that EECP restores endothelial function in patients with coronary insufficiency, certainly a good thing; his study was carried out in Japan. In this paper, Schechter and colleagues repeat Urano's study, here in an Israeli population of inoperable coronary patients with persistent class 3 to 4 symptoms. Their normal range was not given, and may be different from Urano's (different researchers may use different measuring techniques so their "normal" values may be different), but in Schecter's population, just as in Urano's, percent flow mediated vasodilation, the measure of endothelial tone. increased with external counterpulsation, here from 3.5 to 8.2%, coincident with a reduction in average NTG need from 4.7 to 0.4 tabs per day, and an improvement in functional class from 3.3 to 2.0. No matter which continent you use it in, or what you call it (EECP in the US, Asia, and Europe or ECPT in Israel), external counterpulsation works. Endothelial function, the critical predictor of cardiovascular health and outlook, improves, while previously treatment refractory symptoms recede or resolve. The New Therapeutic Approach with the Enhanced External Counterpulsation in Patients with Chronic Stable Angina: Evaluation of Myocardial Flow and Flow Reserve by N-13 Ammonia Pet. Masuda, D, Circulation 100:18 Suppl. 1 Nov. '99 Our most precise indicator of coronary artery blood flow is the PET (Positron Emission Tomography) Scan. Here the scan measures not only blood flow, but the metabolic function of the heart muscle cells supplied with blood and oxygen by a given coronary artery. Dr.Masuda recorded coronary artery flow reserve by the Dipyridamole PET technique, nitric oxide levels, and treadmill time in 11 patients undergoing a 35 hour course of EECP. Treadmill time improved by 49 seconds, or 12%, from 390 to 439 seconds. Time to ST depression, the EKG event reflecting insufficient blood flow to the exercising heart muscle, increased by 185 seconds, essentially doubling, from 190 to 375 seconds. Nitric oxide level doubled, and regional perfusion, the PET indicator of collateral generation, increased in all vascular distributions studied.
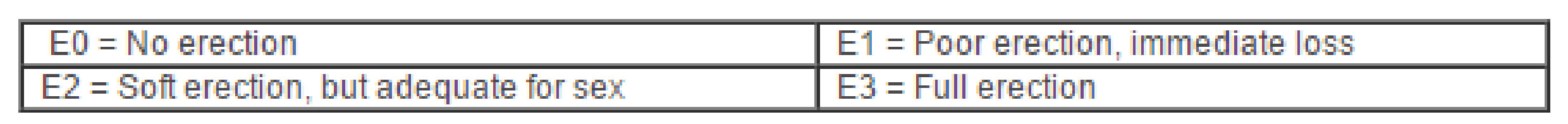
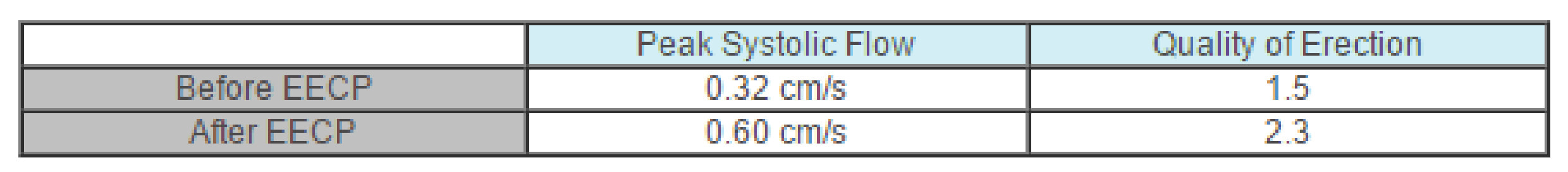
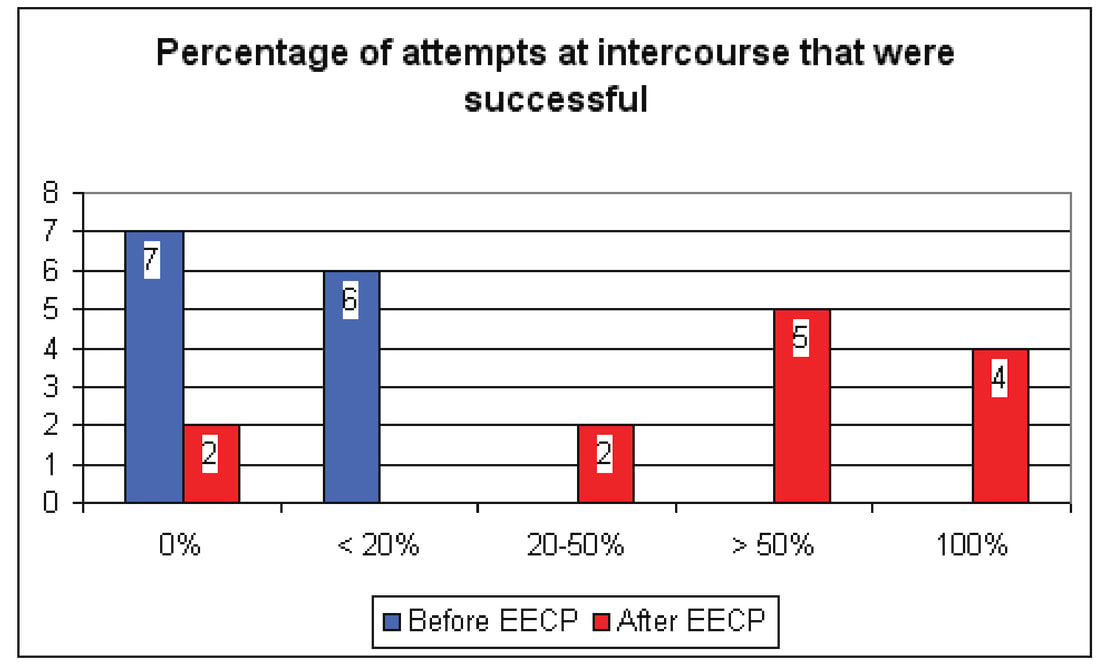
With EECP, collateral vessels are recruited and enlarged, nitric oxide and antioxidant levels rise, renin and endothelin levels fall, PET, Thallium, and stress EKG findings improve, angina decreases and patients feel better. EECP is getting the job done! Enhanced External Counterpulsation as a New Treatment Modality for Patients with Erectile Dysfunction. Froschermaier, S, Urologia Internationalis 1998;61:168-71 Erectile Dysfunction (ED) is essentially endothelial dysfunction, here compromising nitric oxide production and consequent vasodilation within the penile arteriolar system. Viagra works by blocking the breakdown of cGMP, nitric oxide's second messenger, so it stands to reason that measures designed to improve penile endothelial function will help with ED. Arginine supplementation improves overall and penile endothelial function, and helps when ED is vascular in origin. Several papers have documented the nitric oxide generating feature of EECP, and Urano's paper (article 10 û this section) showed us that vascular endothelial dysfunction, as measured by flow mediated brachial artery vasodilation, essentially normalizes following a course of treatment. We know from Werner's paper (article 5 û this section) that blood flow to the pelvic region (internal iliac artery) increases by 140% during an EECP treatment, so we can predict that EECP might be helpful in ED. Fricchione's study (article 5 û section 1), which focused on the effect of EECP on quality of life parameters, noted that love life improved in 1/3 of their subjects following EECP. In this paper, Froscheimer studied the effects of EECP on both subjective and physiologic parameters of erectile function in 13 men with ED. All 13 men had a stable sexual relationship. 6 of the men were diabetic and 12 were cigarette smokers. Physiologic and functional measurements of erectile function were carried out before and 4 weeks after a standard 35 hour course of EECP. Each man graded the quality of erectile function on the following 4-point scale, and recorded the percentage of attempts at intercourse that were successful. As a physiologic measure, peak penile artery blood flow rate was recorded. Froschermaier's findings are presented below is tabular and graphic form. Penile artery systolic flow essentially doubled, and perceived quality of erection on a four-point scale improved from 1.5 to 2.3. Pre-EECP, intercourse was not possible for 7 of the men, and was successful in <20% of attempts in 6. Only 2 of the 13 men did not benefit from EECP; erectile dysfunction improved in 7, while in 4 ED fully resolved. Only 3 of the 13 subjects reported spontaneous morning erections pre-EECP, while post-EECP 11 men noted morning erections. Patients come to us for relief of refractory angina, but they don't mind it a bit when their love life improves.
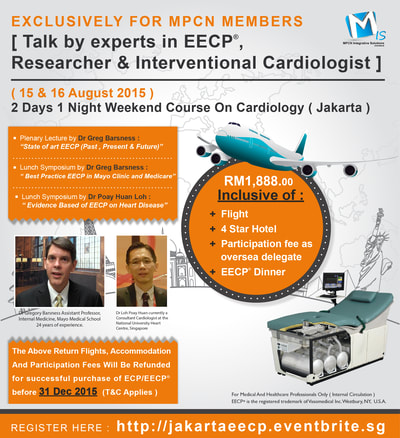
Download Here: www.mpcn.asia/MedicalDeviceAct2012(Eng).pdf
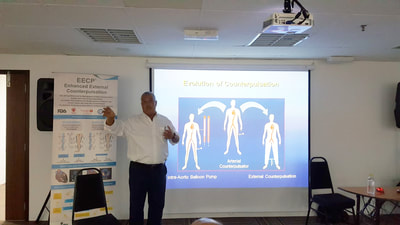
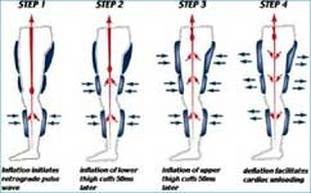
Hearing Loss Pneumatic External Counterpulsation (PECP): A New Treatment Option for Therapy-Resistant Inner Ear Disorders? Offergeld, C, Werner, D, et al Laryngo-Rhino-Otologie û Otologie Abstract L-R-O 9 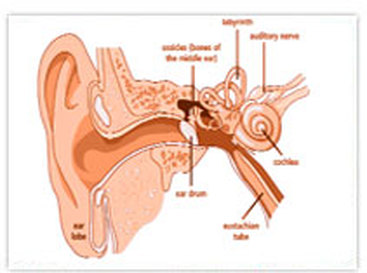 In Germany, the standard therapy for sudden deafness and tinnitus (persistent ringing in the ears) involves drug therapy designed to improve blood flow to the inner ear. Werner's group had previously demonstrated an increase in carotid artery blood flow with EECP (described in Germany as PECP). In this study, 30 patients with acute hearing disorders and/or tinnitus, persisting despite standard drug therapy, received 5-10 one-hour EECP treatments. For the group, internal carotid (front of the brain) and vertebral artery (back of the brain) flow volume, measured by doppler ultrasound, increased during EECP by 19% & 11% respectively. Tinnitus decreased in 47% of the patients, by an average of 16 dB. Hearing threshold increased in 28%, on average by 19dB. Audiometry studies carried out post-treatment demonstrated that the improvement related to EECP persisted throughout a one-year follow-up period. Sudden hearing loss, in certain cases, appears to be related to a reduction in blood flow to the ear and/or the nerves that connect it to the brain. EECP has the potential to increase blood flow to any organ, and to permanently enhance flow via collateral formation. It makes sense that EECP would help here.  EECP is a mechanical procedure in which long inflatable cuffs (like blood pressure cuffs) are wrapped around both of the patient's legs. While the patient lies on a bed, the leg cuffs are inflated and deflated with each heartbeat. This is accomplished by means of a computer, which triggers off the patient's ECG so that the cuffs deflate just as each heartbeat begins, and inflate just as each heartbeat ends. When the cuffs inflate they do so in a sequential fashion, so that the blood in the legs is "milked" upwards, toward the heart. EECP has two potentially beneficial actions on the heart. First, the milking action of the leg cuffs increases the blood flow to the coronary arteries. (The coronary arteries, unlike other arteries in the body, receive their blood flow after each heartbeat instead of during each heartbeat. EECP, effectively, "pumps" blood into the coronary arteries.) Second, by its deflating action just as the heart begins to beat, EECP creates something like a sudden vacuum in the arteries, which reduces the work of the heart muscle in pumping blood into the arteries. Both of these actions have long been known to reduce cardiac ischemia (the lack of oxygen to the heart muscle) in patients with coronary artery disease. Indeed, an invasive procedure that does the same thing, intra-aortic counterpulsation (IACP, in which a balloon-tipped catheter is positioned in the aorta, which then inflates and deflates in time with the heartbeat), has been in widespread use in intensive care units for decades, and its effectiveness in stabilizing extremely unstable patients is well known. While a primitive form of external counterpulsation has also been around for a long time, it has not been very effective until recently. Thanks to new computer technology that allows the perfect timing of the inflation and deflation of the cuffs, and produces the milking action, modern EECP has been greatly enhanced. EECP is administered as a series of outpatient treatments. Patients receive 5 one-hour sessions per week, for 7 weeks (for a total of 35 sessions). The 35 one-hour sessions are aimed at provoking long lasting beneficial changes in the circulatory system.
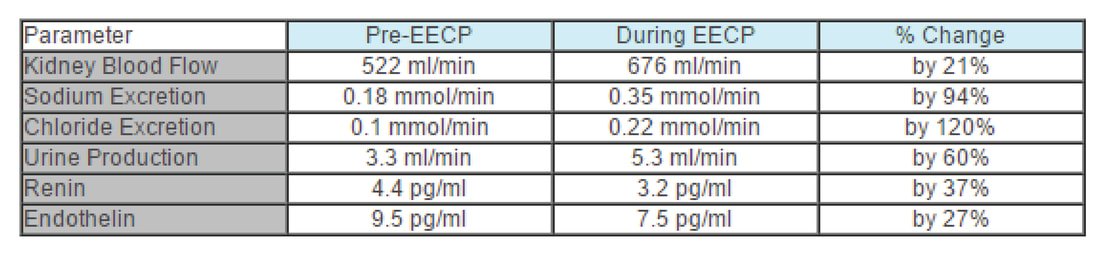
In these patients, the X-ray dye that we use during angiography and angioplasty can sludge up in the kidneys, compromising kidney function further; full blown kidney failure can rarely occur. In this group, we might turn to EECP as a safer means of reducing angina, but we need to be sure that EECP also won't harm the kidneys. Intuitively, one would predict that EECP would have a beneficial effect on kidney function. The American studies discussed above show that EECP increases blood flow to the heart and improves heart function. Blood flows through native arteries, vein grafts, and arterial grafts increases, and heart function, as measured by treadmill time, nuclear scanning, and angina frequency, also improves. Chinese studies tell us that blood flow to the brain increases with EECP, leading to an improvement in brain function in certain patients. Werner and colleagues set out to study the effect EECP has on blood flow to the kidneys and how this might affect kidney function. Using a non-invasive ultrasound technique, Werner measured blood flow to the kidneys before and during EECP in 9 healthy volunteers. Parameters of kidney function were assessed in 12 others. Their findings are summarized in the table and discussed below: A. Blood flow to the kidneys increased by 21%, from 522 to 676 ml/min. This is a positive finding. The more blood presented to the kidney per minute, the better it can do its job of filtering waste products and controlling body water and salt levels.
B. One of the jobs of the kidney is to remove salt from the body, so excretion of the components of salt, sodium and chloride, serve as a measure of kidney function. During EECP, sodium excretion nearly doubled, from 0.18 to 0.35 mmol/min; chloride removal increased likewise from 0.1 to 0.22 mmol/min. C. Urine is composed of body wastes, byproducts of metabolism that have toxic effects if allowed to remain in the body. The kidney filters these waste and excretes them in the urine, so urine production rate serves as a good measure of overall kidney function. Werner found that urine production increased by 60% during EECP, from 3.3 to 5.3 ml/min. This is why you feel the need to empty your bladder during EECP - because your kidneys are working better. D. Renin is a kidney produced hormone that plays a key role in salt and fluid balance and blood pressure control. When renin levels are high, sodium and water are retained, and blood pressure rises. When renin levels are low, sodium and water are excreted, and blood pressure falls. When blood flow to the kidneys is impaired, the kidneys will produce more renin. Salt retention will occur, expanding the blood volume. Blood pressure will rise, increasing blood flow to the kidneys. Blood flow to the kidneys and kidney function will improve, but the rest of the body pays a price. The elevation in blood pressure strains the heart and increases the patient's risk of stroke. The salt and water retention may lead to edema formation or an aggravation of congestive heart failure. When it comes to renin production, the kidney "cares only about itself". This is why patients with poor kidney function or impaired blood flow to the kidneys as a result of cardiovascular disease typically have elevated renin levels, high blood pressure, and a tendency towards fluid retention, edema, and congestive heart failure. On the other hand, when the kidneys are receiving an adequate blood flow, they begin to produce less renin, and good things follow. Blood pressure falls, decreasing stroke risk and the heart's workload. With less fluid retention comes an improvement in edema and a decreased tendency towards CHF. For the cardiac patient, an elevated renin level is bad, and any intervention that lowers renin is to their benefit. During EECP, renin levels fell by 37%, from 4.4 to 3.2 pg/ml. E. Endothelin is nasty stuff. It constricts arteries. It constricts the coronary arteries, compromising blood flow to the heart. It constricts peripheral arteries, raising blood pressure, increasing the heart's workload. We want a low endothelin level, especially if we have coronary artery disease. Werner found that endothelin levels fell by 27% during EECP, from 9.5 to 7.5 pg/ml. To summarize, in healthy volunteers (and presumably in patients), EECP: 1. Increases blood flow to the kidney 2. Improves the ability of the kidney to produce urine 3. Promotes excretion of sodium and chloride 4. Lowers levels of the harmful hormones renin and endothelin |
EECP Therapy in MalaysiaWelcome to our blog section. My name is Alex Wong the Founder and main driver for ECP and EECP therapy in Malaysia. Categories
All
|